Hypoparathyroidism
Parathyroid hormone (PTH) plays a critical role in controlling calcium, phosphate and calcitriol (active vitamin D) levels in the blood and bone. Through its primary actions, PTH directly involves the kidneys, bone and other organs in maintaining key biological functions.1
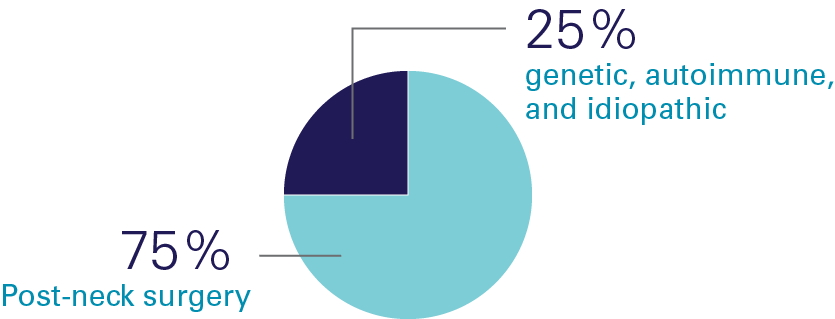
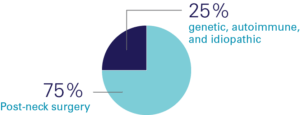
Hypoparathyroidism (also known as hypopara or HP) is a rare endocrine disorder characterized by deficient or absent parathyroid hormone1. It affects over 200,000 people worldwide and a recent review of available data indicated there were approximately 14,000 people affected in the UK, most of whom develop the condition following damage to or accidental removal of the parathyroid glands during thyroid surgery2-4. Current standard of care treatment with calcium and calicitriol (or the analogue alfacalcidol/alphacalcidol) does not effectively address both the short-term symptoms and long-term complications, or the quality-of-life impacts of hypoparathyroidism5-6.
- Mannstadt, M., Bilezikian, J.P., Thakker, R.V., Hannan, F.M., Clarke, B.L., Rejnmark, L., Mitchell, D.M., Vokes, T.J., Winer, K.K. and Shoback, D.M. (2017). Hypoparathyroidism. Nature Reviews Disease Primers, 3(1). doi:https://doi.org/10.1038/nrdp.2017.55.
- Parathyroid UK (n.d.). Hypopara: A quick guide. [online] Parathyroid UK. Available at: https://parathyroiduk.org/hypoparathyroidism/.
- Brandi, M.L., Bilezikian, J.P., Shoback, D., Bouillon, R., Clarke, B.L., Thakker, R.V., Khan, A.A. and Potts, J.T. (2016). Management of Hypoparathyroidism: Summary Statement and Guidelines. The Journal of Clinical Endocrinology & Metabolism, 101(6), pp.2273–2283. doi:https://doi.org/10.1210/jc.2015-3907.
- Mannstadt, M., Bilezikian, J.P., Thakker, R.V., Hannan, F.M., Clarke, B.L., Rejnmark, L., Mitchell, D.M., Vokes, T.J., Winer, K.K. and Shoback, D.M. (2017). Hypoparathyroidism. Nature Reviews Disease Primers, 3(1). doi:https://doi.org/10.1038/nrdp.2017.55.
- Zavatta, G. and Clarke, B.L. (2020). Challenges in the management of chronic hypoparathyroidism. Endocrine Connections, 9(10), pp.R229–R240. doi:https://doi.org/10.1530/ec-20-0366.
- Gosmanova, E.O., Houillier, P., Rejnmark, L., Marelli, C. and Bilezikian, J.P. (2021). Renal complications in patients with chronic hypoparathyroidism on conventional therapy: a systematic literature review. Reviews in Endocrine and Metabolic Disorders, 22(2), pp.297–316. doi:https://doi.org/10.1007/s11154-020-09613-1.
Causes of Hypopara
Burden of disease
People living with hypoparathyroidism experience a diverse range of physical, mental, cognitive and emotional symptoms. They often suffer debilitating symptoms and the condition can severely impact quality of life and overall productivity, including ability to work and perform household activities.
Even worse, the current standard of care with treatment of calcium and calicitriol or the analogue alfacalcidol/alphacalcidol does not fully control the condition, poses a significant daily pill burden, and contributes to risk of long-term complications, including renal disease. People with hypoparathyroidism have at least a four-fold greater risk of kidney failure than the general population, in part due to excessive urinary calcium excretion and long-term complications caused by standard treatment.
Hypoparathyroidism is also linked to increased hospitalizations and emergency room and urgent care visits. In some cases, calcium levels fall so low that patients experience a ‘calcium crash’ and urgently require calcium delivered intravenously – a situation often dreaded by patients, their friends and family.
A survey of people living with hypoparathyroidism (N=146) showed patients required multiple physician visits and up to one decade to diagnose their condition.
A complex patient experience
![]()
Hypocalcemia (low calcium in the blood)1
- Abnormal tingling2, burning2, numbness3 (paresthesia)
- Brain fog (impaired judgment, memory loss, headache)4
- Muscle cramps (tetany)5
- Seizures6
- Laryngospasm (spasm of the voice box)7
Hypercalcemia (too much calcium in the blood)8
- Muscle weakness9, coma10, constipation11, urination difficulties12
Anxiety/fear 13
- May relate to potential calcium crash13
![]()
Calcification
- Calcium deposits in the kidney, brain, blood vessels, eye, and other soft tissues14
Kidney disease
- 4- to 8-fold increased risk of kidney disease compared to healthy populations15
Depression or bipolar disorder
- 2-fold increased risk of depression or bipolar disorder compared to healthy populations16
![]()
Negative psychological impacts
- 100% of patients said their condition interferes with their daily lives
- 85% reported an inability to perform household activities
Negative impacts on the ability to work or work productivity
- 76% reported their condition interfered with work productivity
- 30% were no longer able to work
- Underbjerg, L., Sikjaer, T., Mosekilde, L. and Rejnmark, L. (2015). The Epidemiology of Nonsurgical Hypoparathyroidism in Denmark: A Nationwide Case Finding Study. Journal of Bone and Mineral Research, 30(9), pp.1738–1744. doi:https://doi.org/10.1002/jbmr.2501.
- Khan, A.A., Bilezikian, J.P., Brandi, M.L., Clarke, B.L., Gittoes, N.J., Pasieka, J.L., Rejnmark, L., Shoback, D.M., Potts, J.T., Guyatt, G.H. and Mannstadt, M. (2022). Evaluation and Management of Hypoparathyroidism Summary Statement and Guidelines from the Second International Workshop. Journal of Bone and Mineral Research, 37(12), pp.2568–2585. doi:https://doi.org/10.1002/jbmr.4691.
- Martel, J. (2012). Everything You Need to Know About Hypoparathyroidism. [online] Healthline. Available at: https://www.healthline.com/health/endocrine-health/hypoparathyroidism#causes [Accessed 30 Apr. 2025].
- Shoback, D.M., Bilezikian, J.P., Costa, A.G., Dempster, D., Dralle, H., Khan, A.A., Peacock, M., Raffaelli, M., Silva, B.C., Thakker, R.V., Vokes, T. and Bouillon, R. (2016). Presentation of Hypoparathyroidism: Etiologies and Clinical Features. The Journal of Clinical Endocrinology & Metabolism, 101(6), pp.2300–2312. doi:https://doi.org/10.1210/jc.2015-3909.
- Shoback, D.M., Bilezikian, J.P., Costa, A.G., Dempster, D., Dralle, H., Khan, A.A., Peacock, M., Raffaelli, M., Silva, B.C., Thakker, R.V., Vokes, T. and Bouillon, R. (2016). Presentation of Hypoparathyroidism: Etiologies and Clinical Features. The Journal of Clinical Endocrinology & Metabolism, 101(6), pp.2300–2312. doi:https://doi.org/10.1210/jc.2015-3909.
- Sikjaer, T., Eskildsen, S.F., Line Underbjerg, Østergaard, L., Lars Rejnmark and Lars Evald (2024). Hypoparathyroidism: changes in brain structure, cognitive impairment, and reduced quality of life. Journal of Bone and Mineral Research, [online] 39(7), pp.855–866. doi:https://doi.org/10.1093/jbmr/zjae063.
- Underbjerg, L., Sikjaer, T., Mosekilde, L. and Rejnmark, L. (2015). The Epidemiology of Nonsurgical Hypoparathyroidism in Denmark: A Nationwide Case Finding Study. Journal of Bone and Mineral Research, 30(9), pp.1738–1744. doi:https://doi.org/10.1002/jbmr.2501.
- Shoback, D.M., Bilezikian, J.P., Costa, A.G., Dempster, D., Dralle, H., Khan, A.A., Peacock, M., Raffaelli, M., Silva, B.C., Thakker, R.V., Vokes, T. and Bouillon, R. (2016). Presentation of Hypoparathyroidism: Etiologies and Clinical Features. The Journal of Clinical Endocrinology & Metabolism, 101(6), pp.2300–2312. doi:https://doi.org/10.1210/jc.2015-3909.
- Rubin, M.R. (2020). Recent advances in understanding and managing hypoparathyroidism. F1000Research, 9, p.766. doi:https://doi.org/10.12688/f1000research.22717.1.
- Mayo Clinic (2024). Hypercalcemia - Symptoms and causes. [online] Mayo Clinic. Available at: https://www.mayoclinic.org/diseases-conditions/hypercalcemia/symptoms-causes/syc-20355523.
- Mayo Clinic (2024). Hypercalcemia - Symptoms and causes. [online] Mayo Clinic. Available at: https://www.mayoclinic.org/diseases-conditions/hypercalcemia/symptoms-causes/syc-20355523.
- Zavatta, G. and Clarke, B.L. (2020). Challenges in the management of chronic hypoparathyroidism. Endocrine Connections, 9(10), pp.R229–R240. doi:https://doi.org/10.1530/ec-20-0366.
- Mayo Clinic (2024). Hypercalcemia - Symptoms and causes. [online] Mayo Clinic. Available at: https://www.mayoclinic.org/diseases-conditions/hypercalcemia/symptoms-causes/syc-20355523.
- Khan, A.A., Bilezikian, J.P., Brandi, M.L., Clarke, B.L., Gittoes, N.J., Pasieka, J.L., Rejnmark, L., Shoback, D.M., Potts, J.T., Guyatt, G.H. and Mannstadt, M. (2022). Evaluation and Management of Hypoparathyroidism Summary Statement and Guidelines from the Second International Workshop. Journal of Bone and Mineral Research, 37(12), pp.2568–2585. doi:https://doi.org/10.1002/jbmr.4691.
- Mannstadt, M., Bilezikian, J.P., Thakker, R.V., Hannan, F.M., Clarke, B.L., Rejnmark, L., Mitchell, D.M., Vokes, T.J., Winer, K.K. and Shoback, D.M. (2017). Hypoparathyroidism. Nature Reviews Disease Primers, 3(1). doi:https://doi.org/10.1038/nrdp.2017.55.
- Mannstadt, M., Bilezikian, J.P., Thakker, R.V., Hannan, F.M., Clarke, B.L., Rejnmark, L., Mitchell, D.M., Vokes, T.J., Winer, K.K. and Shoback, D.M. (2017). Hypoparathyroidism. Nature Reviews Disease Primers, 3(1). doi:https://doi.org/10.1038/nrdp.2017.55.
- Khan, A.A., Bilezikian, J.P., Brandi, M.L., Clarke, B.L., Gittoes, N.J., Pasieka, J.L., Rejnmark, L., Shoback, D.M., Potts, J.T., Guyatt, G.H. and Mannstadt, M. (2022). Evaluation and Management of Hypoparathyroidism Summary Statement and Guidelines from the Second International Workshop. Journal of Bone and Mineral Research, 37(12), pp.2568–2585. doi:https://doi.org/10.1002/jbmr.4691.